Lung transplant patient finds strength in numbers
LEXINGTON, Ky. (Nov. 25, 2025) — If you ask Steve Worrell what word describes him, he’ll say this, without hesitation: “Blessed.”
“God has blessed me in may ways, especially when I needed a lung transplant,” he said.
A resident of Richmond, Kentucky, Worrell has been retired for 18 years and spends his time traveling all over the country with Janice, his wife of 25 years. From trips out West to their winters in Florida and everywhere in between, the Worrells are always on the move. As soon as they wrap up one trip, they already have another one planned.
“We love to travel,” Worrell said. “We’re an active couple and we have a large social circle of friends. We do a lot of things with them, whether it be travel, or playing games or having dinner.”
For nearly 20 years, they’ve been on the go — except for a brief pause when Worrell suddenly needed a lung transplant.
‘I couldn’t breathe.’
In 2020, Worrell was diagnosed with pulmonary fibrosis, a disease in which the lung tissue becomes damaged and scarred. Over time, the stiffness of the tissue makes it harder for the lungs to work properly. Worrell can pinpoint the exact moment, five years ago, when he knew something was wrong. The act of doing a small favor for a neighbor became an indelible memory.
“In April of 2020, I saw a neighbor across the street had eight bags of leaves gathered up to be thrown in the trash truck when it came by,” he said. “I just happened to be outside when the trash truck came. So, I skipped over there, and I threw those eight bags into the truck for the driver. It didn't take me 90 seconds to do that, but by the time I got done, my chest was killing me and I couldn't breathe. First time in my life I’d ever experienced anything like that.”
Worrell had always been an active guy — he golfed once or twice a week, played softball, racquet ball, and tennis in his younger years, regularly mowed his lawn and did household chores. He and Janice often took long walks in addition to their travel adventures.
“I was active, but not what you call an athlete,” Worrell said. “I had no aerobic problem at all.”
His primary care physician referred him to a pulmonary specialist who diagnosed him with idiopathic pulmonary fibrosis (IPF). The term “idiopathic” means the disease is spontaneous, and the cause is unknown. Worrell had been healthy and active throughout his entire life; this IPF came out of nowhere.
“Pulmonary fibrosis affects about 1 in 200 adults over age 60,” said Naureen Narula, M.D., transplant pulmonologist and medical director of the Transplant Clinic at UK HealthCare. “At UK, we see roughly 100-150 new cases each year through our interstitial lung disease and transplant clinics. It can result from autoimmune diseases, environmental exposures, medications or sometimes has no known cause.”
For four years, Worrell took a medication called Esbriet, which slowed the progression of his lung disease. He carried on with his yard work, golf games and traveling, putting his lung disease in the back of his mind.
‘It was just that quick.’
That all changed in June 2024, when Worrell suddenly found himself short of breath. By July, he relied on an oxygen concentrator, a device that filters out gases from the air and delivers a higher concentration of oxygen.
“By the end of July, I couldn’t take a shower without wearing 10 liters of oxygen,” Worrell said. “It was just that quick. In a month and a half, I went from a normal life to needing 10 liters of air in the shower.”
“Sometimes the disease can take a sudden turn,” said Narula. “In Mr. Worrell’s case, an acute flare caused his lungs to stiffen quickly, making it hard for him to breathe despite all the right treatments. It’s something we unfortunately see in a small percentage of patients. This flare can often be triggered by infections or inflammation, even when they’ve been stable before.”
By the end of August, Worrell was admitted to the intensive care unit at the UK Albert B. Chandler Hospital. On Sept. 13, 2024, he was put on the list for a lung transplant. At this point, Worrell was at 70% oxygen; without sufficient oxygen, he was at risk for potentially fatal organ failure.
“The more oxygen he received, the higher he went on the list,” said Janice. Her husband — who only weeks prior was golfing with friends — was on the verge of needing ventilator, a machine that would breathe for him when his lungs could no longer support him. Narula estimates that about 10-15% of patients with advanced pulmonary fibrosis eventually require a transplant when medication can no longer control the disease.
Three days later, Janice got the call — Narula and the transplant team had found a lung for her husband. The shortness of his wait correlated directly to his rapidly deteriorating condition, but the overall criteria for considering a patient for transplant is complex. Nationwide, there is a shortage of donor organs for patients like Worrell who are in the end stages of lung disease. Many factors are considered, including the prior health of the patient. And at 73, Worrell had been in excellent health.
“We now know that the biological age matters more than the chronological age,” said Narula. “With advances in surgery and post-transplant care, many patients in their 70s recover well and thrive after transplant. Today, we focus on a person’s overall health and fitness, not just their chronological age. He was highly motivated, physically strong for his age, and had excellent family support — all key factors for success after transplant.”
Whether a patient has a strong support system is also a key factor in determining a patient’s eligibility for transplant. That’s something Worrell had in abundance. Family and friends had started prayer chains for him, with prayer warriors in as many as six states.
He counts his friends Bob and Jan as key members of his care team.
“We've got a large circle of family and friends, and they all wanted to help,” Worrell said. “But not everybody has the time or the physical ability to push a guy like me around in a wheelchair all over UK. We could put in miles going around from test to test with my friend Bob pushing me in a wheelchair. Jan carrying my records and Janice just attending to whatever's going on. They went with us every trip and every step of the way.”
‘Everything’s gone great since.’
At 1:30 a.m. Sept. 18, 2024, Worrell’s transplant team, led by surgeon Matthias Loebe, M.D., performed a single lung transplant. For patients over 70 like Worrell, a single lung transplant is a more common approach for older adults because of the shorter surgery and recovery time; outcomes are similar to those who receive a double lung transplant.
Before her husband was wheeled away to the operating room, Janice hatched a plan.
“I told Steve prior to the surgery that when you get back to the room and I come see you, I’m going to twist your big toe so you know it’s me,” Janice said. “I go in; he’s laying there with all these machines hooked to him. I get to the foot of the bed, and I twisted his big toe. And you know what he did? He winked at me. One of his nurses said, ‘Okay, he’s doing good. He’s already flirting with his wife.’ That meant so much to me. I’ll never forget that.”
After the breathing tube was removed, Worrell took a few unsteady breaths.
“It’s hard to breathe deep when you’re not used to breathing deeply,” he said. “That’s what I remember — being afraid to breathe deep.”
He quickly vanquished that fear, rallied his strength and was on his feet in no time. Three weeks after his friend Bob wheeled him into the hospital, and eight days after his transplant, Steve Worrell walked out the front door of UK Chandler Hospital. And he hasn’t stopped moving since.
After the requisite post-transplant recovery and isolation period where he needed to avoid crowds and stay close to the hospital, he and Janice picked right back up where they left off. Three months after his surgery, they went for a hike at Cumberland Falls. Six months after that, they flew to Jackson, Wyoming, to celebrate his recovery with his family.
Narula, Loebe and the rest of the UK Transplant Team attribute Worrell’s recovery to his pretransplant health and stamina. That’s part of it, Worrell said, but having a strong system of support — a close circle of family and friends — is crucial to a successful outcome.
“I want other transplant patients to know how important it is to have that care team at home after being discharged from the hospital,” he said. “I'm a blessed guy that I was healthy going in and healthy coming out. I'm an organized person. I stay on top of detail. A lot of people aren't healthy enough to do all that, and they need that good care team. The care team can make being a patient so much easier.”
Beyond their family and social circle, the Worrells have developed personal bonds with his UK HealthCare team, one that transcends the patient/provider relationship. At Christmas and on Valentine’s Day, he and Janice delivered cookies and treats. On the one-year anniversary of his surgery, they visited the post-transplant recovery floor with a giant “1” balloon to celebrate the milestone with those who were there at the beginning.
“Dr. Narula, Dr. Loebe, Dr. Anstead, the pharmacists, the phlebolomy techs, phlebotomy aides, the respiratory therapists, the office administration — We feel like they’re family to us,” he said.
For Narula, the feeling is mutual.
“They’re an incredible, optimistic couple — grateful, hardworking and deeply committed to recovery,” she said. “Their teamwork has been inspiring to our whole team. Lung transplantation offers people with advanced lung disease a second chance at life, and stories like Mr. Worrell’s reminds us why this work matters every day.”
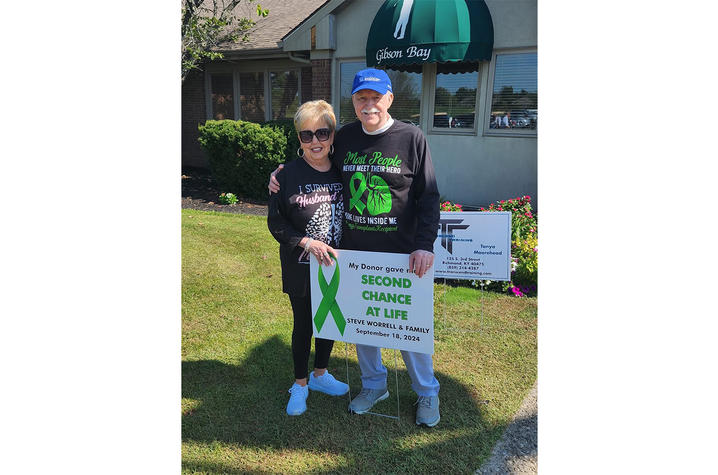
More than a year after his transplant, Worrell is looking for ways to give back. He recently participated in the Second Chance at Life golf scramble, raising nearly $8,000 for the organization to promote organ donation and support patients and their families. In a photo, Worrell’s shirt sums up the gratitude he has for the anonymous donor who gave him a second chance at life, and more years to spend with his family and friends.
“Some people never meet their heroes,” the shirt reads. “Mine lives inside me.”
UK HealthCare is the hospitals and clinics of the University of Kentucky. But it is so much more. It is more than 10,000 dedicated health care professionals committed to providing advanced subspecialty care for the most critically injured and ill patients from the Commonwealth and beyond. It also is the home of the state’s only National Cancer Institute (NCI)-designated Comprehensive Cancer Center, a Level IV Neonatal Intensive Care Unit that cares for the tiniest and sickest newborns and the region’s only Level 1 trauma center.
As an academic research institution, we are continuously pursuing the next generation of cures, treatments, protocols and policies. Our discoveries have the potential to change what’s medically possible within our lifetimes. Our educators and thought leaders are transforming the health care landscape as our six health professions colleges teach the next generation of doctors, nurses, pharmacists and other health care professionals, spreading the highest standards of care. UK HealthCare is the power of advanced medicine committed to creating a healthier Kentucky, now and for generations to come.