Barnstable Brown Diabetes Center Patient is First in Lexington to Use Latest Insulin Pump Technology
LEXINGTON, Ky. (April 3, 2018) – No matter how diligently a person with diabetes works at their diabetes management, the amount of effort put in doesn’t always yield the desired results, and it can be very frustrating.
A person living with diabetes can spend hours every day tracking blood glucose levels, calculating insulin injections, finding time for exercise, counting carbohydrates and making food substitutions. Timing is everything in all areas of life, particularly for the person living with diabetes. The challenges can be great but the reward of a longer, healthier life is greater.
Advances in diabetes management continually improve and an insulin pump has been an option for many patients. Insulin pumps administer insulin subcutaneously and must be programmed according to blood glucose levels and food intake. The pump requires one needle stick every two to three days to deliver the insulin through a cannula attached to the pump versus daily multiple injections with a syringe. Wearing a pump can simplify the demands of diabetes management for many people.
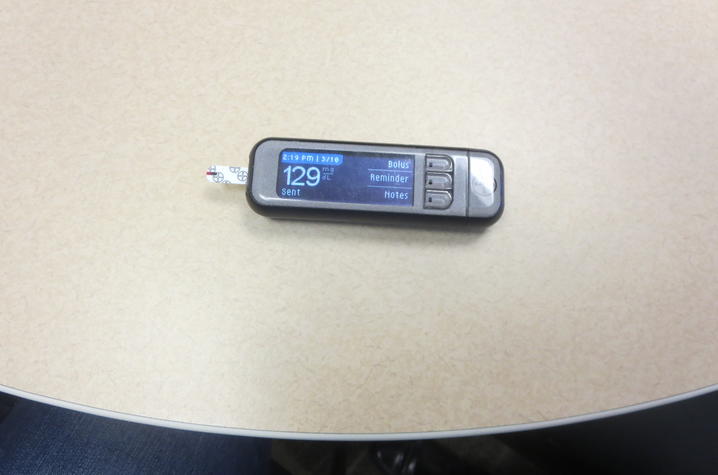
The University of Kentucky Barnstable Brown Diabetes Center now offers an insulin pump that allows patients even more freedom and control. The Medtronic 670G Closed Loop Hybrid insulin pump is the first and only technology that mimics some of the functions of a healthy pancreas by automatically delivering a personalized amount of insulin 24-hours a day. Basically, after the first week or two of wear, the pump “learns” the patient and creates a set of algorithms that change the insulin dosing as the patients’ needs change, offering less blood sugar fluctuations and improved overall glycemic control. In July 2017, Lisa Conley, a BBDC patient from Richmond, Kentucky, became the first person in Lexington and the first person at Barnstable Brown to wear the new technology. Her experience using the 670G has created a knowledge base for her providers and for BBDC patients who came after her to wear the 670G.
Lisa’s story
Lisa Conley, 52, spent the better part of her adult life in the health care industry in one capacity or another so she knew the importance of being proactive and taking care of herself when she was suddenly diagnosed with type 1 diabetes in her early 30s.
The mother of a 2-year-old and a 9-month-old infant, Conley lived in Iceland at the time with her husband who was in the military. Even with her symptoms of sickness and weight loss, she was still shocked by her diagnosis since she had no symptoms prior to this time. She has no idea what her medical history might be because she was adopted as an infant.
While living in Iceland and working as a medical technologist, she had a strong support system with her diabetes care and education. She managed well on four shots a day. She and her family eventually transferred to Camp David at Bethesda, Maryland, and a few years later to Pensacola, Florida. While in Florida, she shifted career paths and began to travel internationally for a health care company that sold software to hospitals. Conley stayed on top of her diabetes management juggling a busy life as a wife and mom with a demanding career.
Four insulin injections a day became more of an inconvenience the more she traveled internationally. Conley began reading the literature on insulin pumps and doing her own research. By the time her husband retired from the military in April 2006, she decided an insulin pump would make traveling much easier.
Conley’s doctor in Florida advised her that the best place in Kentucky for her diabetes care would be the BBDC at UK. It was here that Conley started using her first insulin pump. She upgraded several times over the years as improved models were released. The pumps did give her more freedom and control although she still had to do finger sticks five to six times a day to program into her pump.
Insulin pumps are not new. The first pump was developed in 1963 by a California physician and was about the size of a microwave, designed to be worn like a backpack. Over the years, pumps became more proficient and gradually decreased in size to that of a small pager.
Since coming to Kentucky and the BBDC, Conley has forged a strong working relationship with her physician, Dr. Lisa Tannock, and her diabetes care team.
“The comprehensive care offered by BBDC is critical to the success of patients like Lisa. It is our team of physicians, advanced practice providers, diabetes educators, and staff that allows us to provide cutting edge care,” Tannock said.
There are times, despite best efforts, that things like diabetic ketoacidosis (DKA) occurs and it happened to Conley, which landed her in UK’s emergency department. DKA is a dangerous build-up of acids in the blood due to the lack of insulin. This was a frightening experience for Conley but what stands out most about that experience is the attentiveness and care that Dr. Tannock and her team gave her.
Always one to keep up on the latest technology, Conley studied the literature on the latest Medtronic 670G Hybrid Closed-Loop system, currently the only pump that constantly self-adjusts to automatically keep glucose levels in target range, based on how patients live their lives. Hence, the term “closed-loop” meaning the continual communication between the pump and the patient’s algorithms requires less input from the patient since much is done automatically. The patient is still responsible for giving the pump information about carbohydrate intake and high blood sugars for the pumps algorithms to adjust.
The pump personalizes to the patient in two ways: 1) a suspend before low feature that avoids low glucose levels and rebound high levels by suspending insulin 30 minutes before pre-selected low limits are reached, then automatically restarts insulin once glucose levels recover without intrusive alerts; and 2) the auto mode option that automatically adjusts basal insulin delivery every five minutes based on sensor glucose levels to keep patients in target range day and night.
When Conley told her Barnstable Brown care team she wanted to try the Medtronic 670G, it coincided with the BBDC introduction of the 670G to their patients. They enthusiastically supported her willingness to embrace the new technology in the very early days of introduction
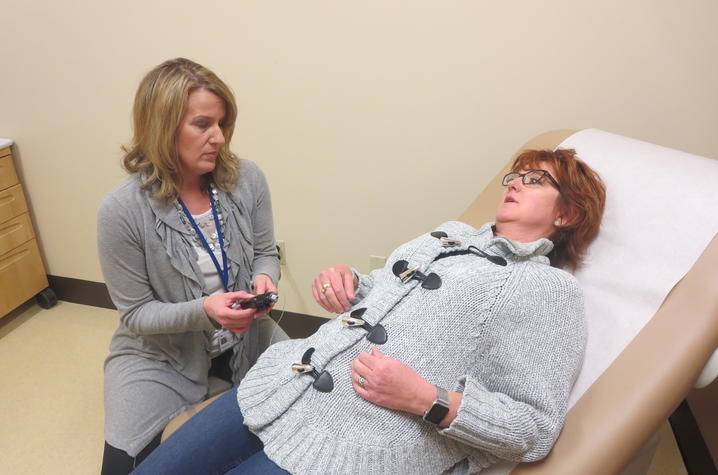
“We learn as much from her as she does from us,” said Sheri Setser-Legg, Diabetes Education Service Coordinator at BBDC. “We’re very fortunate to be at a research institute like UK and have patients like Lisa who are willing to try the latest technology.”
Setser-Legg says that BBDC currently has 25 to 30 adult patients and one or two pediatric patients on the 670G pump.
“I can’t imagine my life without this pump; it is far superior to shots,” Conley said.
The Barnstable Brown Diabetes Center serves the Commonwealth of Kentucky for diabetes management and offers comprehensive evaluations and treatment plans. Physicians work alongside other providers in managing the care of patients with diabetes by providing support and assistance as needed. For patients requiring intensive management, such as patients using insulin pumps, patients with type 1 diabetes, and patients with challenging diabetes issues, in-depth care is provided on an ongoing basis.
Kentucky has the 4th highest diabetes mortality rate in the nation, In Kentucky, diabetes is the 6th leading cause of death by disease overall, and the 5th leading cause of death by disease for African-Americans. Significant risk factors associated with uncontrolled diabetes include blindness, amputation, and kidney failure.
The American Diabetes Association estimates that diabetes cost Kentucky nearly $4 billion in total medical costs, lost work and wages. People with diabetes nationally have cost 2.3 times higher than would be expected in its absence.