UK HealthCare team offers care, wraparound support for endocarditis patients
LEXINGTON, Ky. (March 19, 2024) — A devastating car crash left then 19-year-old Joshua Gilvin with a fractured spine and a prescription for a pain medication containing oxycodone.
“I found myself abusing them a little bit,” Gilvin said. “Next thing you know I’m going to have my teeth pulled and everything to get a pill.”
That included driving as far as Florida to get a prescription filled. When the pills got too expensive, he began to use heroin and other substances that could be injected with a needle. Gilvin spent years estranged from family and without steady housing.
In 2016, Gilvin was diagnosed with endocarditis — a life-threatening heart infection. The infection can occur naturally but drug use with a contaminated needle can put someone at greater risk for the disease. At 34, Gilvin had his first open heart surgery.
Now 42, the Bath County native has been in recovery from opioid use disorder for more than three years. Thanks to the care of his providers at UK HealthCare, Gilvin lives with a mechanical heart valve and a pacemaker.
“Who would have thought at 42 years old I’d have two heart surgeries and a pacemaker? That’s crazy,” Gilvin said. “But my kids love me now.”
His story is not unique.
The rise of the opioid epidemic has fueled a rise in younger, sicker endocarditis patients — a challenge for hospitals accustomed to lower incidence of the potentially deadly disease. But UK HealthCare’s multidisciplinary endocarditis team, launched in 2021, has responded to the challenge.
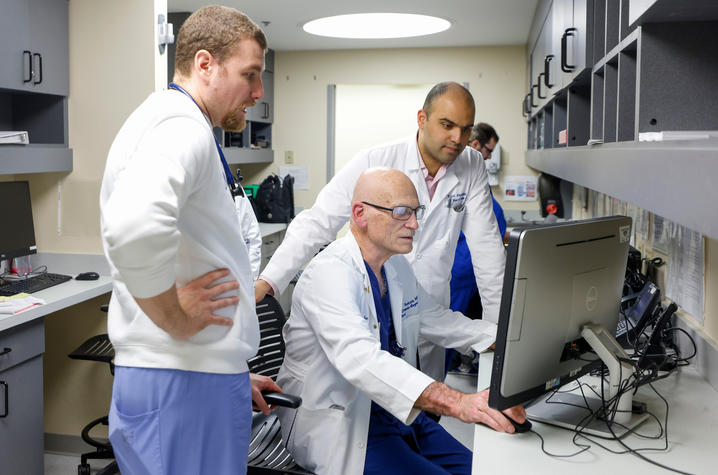
From cardiac surgeons to social workers, the team brings together a wide variety of UK HealthCare experts for a common goal: Lowering mortality rates for endocarditis patients.
“It's a very complicated disease,” said Sami El-Dalati, M.D., infectious disease physician and director of UK’s multidisciplinary endocarditis team. “It requires input from a lot of different specialties.”
'A massive explosion’
A recent study published in the Journal of the American Heart Association found an increase in endocarditis-related deaths among 25 to 44-year-olds between 1999 and 2020. Kentucky and other states close to the epicenter of the opioid crisis have seen significant increases.
A study of endocarditis patients coming to UK HealthCare over a 10-year period identified a “massive explosion” in endocarditis cases related to drug use, El-Dalati said. Between 2009 and 2010 the hospital saw 75 endocarditis cases, and 38% were related to drug use.
“Then, by 2017-2018, in those two years there were 505 cases, and three-quarters of them were from drug use,” El-Dalati said. “So it just really exploded, and they were really overwhelmed with endocarditis.”
Enter the need for a coordinated endocarditis team. The team grew organically among physicians, and the arrival of El-Dalati — who was previously a part of a similar team at the University of Michigan — was key.
“Before Dr. El-Dalati came, we had no structure and I would always see these patients again in my clinic,” said Michael Sekela, M.D., chief of cardiothoracic surgery and a member of UK’s endocarditis team. “But a lot of times when they had an operation, or an intervention, or even discharge from the hospital, there was no long-term plan about how to look after them.”
The multidisciplinary team meets weekly to discuss the hospital’s endocarditis patients and their care. A diverse range of experts from specialties like infectious disease, cardiology, cardiac surgery, addiction medicine, palliative care and physical medicine and rehabilitation join the meeting to offer input on endocarditis patient care from the moment they enter the hospital to continued follow-up care months after discharge.
If a certain case demands it, some other specialties like neurology or neurosurgery are also called on to offer input.
“I find this work to be incredibly meaningful and restorative, particularly with combating burnout,” El-Dalati said. “It’s such a privilege that patients put their trust in us to guide them through these incredibly challenging times in their lives and what I am so proud of about our team is that I think everyone takes that very seriously. Part of what has been missing for this population is trust in the health care system and one of our missions is to try and rebuild that trust.”
The team treats all of the hospital’s endocarditis patients – about half of which are related to drug use, El-Dalati said.
“We follow some of our patients (like Mr. Gilvin) for years,” El-Dalati said. “Even though not all of our patients survive, sometimes just creating a trusting patient-provider relationship is a meaningful intervention by itself. All of our team members volunteer their time to this endeavor and every week the meeting is a reminder of how committed each person is to caring for others and, for me personally, encourages me to keep persevering.”
Only a handful of hospitals nationwide have similar teams. In a region that has deeply felt the family and community damaging effects of the opioid crisis, UK’s endocarditis team is a resource for the Commonwealth. UK HealthCare’s in-hospital mortality rate for endocarditis is down to 9.9% from 17.6% in 2017-2018.
“What we have at UK is pretty unique and novel,” El-Dalati said. “Even the other places that have these programs don't do as much of the outpatient care, like the multidisciplinary clinics, the nursing support.”
Life on the move
The car crash that changed Gilvin’s life happened on Sept. 8, 2001. He remembers watching the 9/11 attacks on TV three days later, unable to move from the couch because of his injuries.
“From that day on,” Gilvin said, “my life spiraled out of control.”
That life was often on the move. Trips to Florida brought back more than 1,000 pills at a time. Then trips to Virginia, Tennessee or Ohio followed as the supply tightened and prescriptions got harder to fill.
Eventually, a cousin — who Gilvin no longer talks to — offered him heroin acquired in Cincinnati. Soon time was split between hours of “hiding out” high in the bathroom and trips north to Cincinnati.
“No kind of life to live,” Gilvin said. “It got so bad we were doing meth, too.”
Grandparents started raising his two kids. Gilvin and his girlfriend were using multiple substances before she eventually left. He spent nearly seven years without steady housing, “bouncing around tent-to-tent, couch-to-couch.”
During a stint in jail, Gilvin began to feel sick. Eventually he was taken to a Lexington hospital and given his frightening endocarditis diagnosis — requiring his first open heart surgery to repair a heart valve plus a six-week stay. For Gilvin, it was both scary and constricting.
“I was so used to running all the time, you know, on the road, go, go, go,” Gilvin said. “So sitting in the hospital for six weeks really wasn't an option.”
An opportunity to support
Gilvin stuck it out. But that first trip to the hospital for endocarditis patients can often be a jarring experience, said Alyssa Tremblay, a clinical social worker with UK HealthCare who is also a part of the multidisciplinary endocarditis team.
Many patients don’t make it into the hospital until they’re already quite sick even if they’re young and look “baseline normal” upon first meeting, Tremblay said.
“They're gravely, gravely ill,” Tremblay said. “I think that also makes them tricky to treat, because they come in and they can walk around, but they're being told they have to stay in the hospital for six weeks for treatment of a life-threatening condition. It's hard for them, it's hard for the staff. The reality of that is it’s really hard to wrap your head around how scary it is.”
Social workers like Tremblay work with endocarditis patients from the moment they enter the hospital to well beyond discharge. Tremblay is a member of UK’s Addiction Consult and Education Services (ACES) — a different, hospital-wide multidisciplinary team that offers education to both providers and patients on substance use disorder.
The ACES team also works to counter the negative social stigma that can follow someone suffering from substance use disorder even in health care settings. Simply labeling someone an “addict” is unhelpful and lacks context, Tremblay says.
“No one really likes to say, ‘Well, this person with this chronic disease of substance use also has this 20-year history of trauma, houselessness, poverty and a system that doesn't support them,’” Tremblay said. “Now they're here, and we have this unique opportunity to try to support them with a whole-person approach.”
The patient-centered care the ACES team offers includes prescribing medications like buprenorphine (name brand Suboxone) that help treat opioid dependence. They also can set patients up with various strategies to cope with distress or other therapies that might help make someone more comfortable.
“Substance use disorders are complex treatable diseases, and through the work of this team, we are able to provide not only medical intervention in the time we have together, but also housing stabilization, residential treatment referral, SNAP benefit activation for stable nutrition, transport assistance, replaced government documents, mental health services, safer use coaching and linkage to recovery communities,” Tremblay said. “We meet them where they are and try to do what we can to prevent recurrences of these infections.”
The endocarditis team works closely with UK’s Wrap Around for Addiction and Infectious Diseases program which offers wraparound services and case management for patients after discharge. They call patients to check in and have funds to pay for gas cards or taxis if someone needs help with transportation.
“Did you go to your doctor's appointment? Did you know you have a doctor's appointment tomorrow? Do you need a ride? Do you have food in your house?” said Tremblay, offering examples of what a patient might be asked. “You know, whatever it is that you need.”
It’s important for endocarditis patients to keep up with follow-up appointments. El-Dalati offers combined clinics with cardiac surgeons so patients can see both at once. They can also treat hepatitis C and prescribe medications like Suboxone.
“One of the challenges we have is just keeping them engaged in care and preventing subsequent infections, or, if they've had a surgery, making sure they follow up,” El-Dalati said. “That can be a challenge.”
'My kids won’t even know I’m gone’
After his December 2016 heart surgery, Gilvin went “back out, back to jail, back to the streets, back to torturing myself. Poking and stabbing, can’t find a vein.”
“I was homeless and just giving up on everything,” Gilvin said. “My sister got married, and I didn't even go to her wedding. I was ashamed to be there. Mom wouldn't let me come to Christmas. She wouldn't let me come to Thanksgiving.”
Sometime in 2020, Gilvin was on another six-week hospital stay when he got a life-changing call. His daughter, his “baby girl” wanted to change her last name, Gilvin was told.
“Because I hadn’t been around, she hadn’t seen me,” Gilvin said. “She wanted to have her name changed to her mom’s last name. Man, it struck a chord with me.”
Gilvin kicked his “needle habit” and started on the long road of rehab for help with other substance abuse. Meanwhile, he battled osteomyelitis — a bloodborne, bone infection that can arise from IV drug use – and was making multiple trips to UK HealthCare.
Tessa London-Bounds, M.D., cardiothoracic surgeon in UK’s Gill Heart & Vascular Institute and a member of the endocarditis team, performed a large debridement of Gilvin’s breastbone and collar bone.
The surgery removed sections of those bones to get the osteomyelitis infection under control, London-Bounds said. While the procedure added risk and complexity to the case, it was necessary to help Gilvin get to a place where he could have another heart surgery.
During a 30-day rehab program in Elizabethtown, Gilvin relapsed after another patient brought in “dope.” He admitted what he had done and, after a vote, Gilvin could stay – something he’s thankful for because he had a revelation.
“I'm not going to make it if I don't stay clean,” Gilvin said. “If I don't keep my mind right, I'm going to die out here. I'm going to die alone. My kids won’t even know I’m gone.”
He needed another heart surgery, specifically a new mechanical heart valve — a procedure typically only offered to patients who have demonstrated a commitment to sobriety. After maintaining his commitment for a time, Gilvin got the surgery.
The valves of the heart function somewhat like saloon doors between the heart’s chambers, explained London-Bounds. Infections tend to build up on or damage these valves.
“Anytime that heart beats, those valves open and close, and so if you have a piece of infection on them, essentially, that piece can flick off and it can cause a lot of downstream problems,” London-Bounds said. “It can cause strokes, it can cause infection in all of the other organs in your body, it can also compromise the function of your heart.”
Gilvin’s surgery removed the infection from his heart. He was told that there was a clump on his heart valve that could’ve killed him had it moved. Dr. Sekela, who performed the surgery, told Gilvin it was a “miracle” he was still alive, Gilvin says.
He goes to Christmas dinner now. Gilvin’s mom calls him near-daily to check in. He’d be “lost” without her, Gilvin said. His daughter doesn’t want to change her name anymore.
“I've reconnected with my dad, all my sisters, they all support me now,” he said. “Anything that has to be done, they jump right in.”
The multidisciplinary endocarditis team has plans to expand their outpatient work throughout the state. In February, El-Dalati made the first of several monthly visits to see patients at the UK North Fork Valley Community Health Center in Hazard.
“The charter of UK says, we need to take care of the people of Kentucky,” Sekela said. “My whole career, that's what I go to. That's why we need to do it.”
UK HealthCare is the hospitals and clinics of the University of Kentucky. But it is so much more. It is more than 10,000 dedicated health care professionals committed to providing advanced subspecialty care for the most critically injured and ill patients from the Commonwealth and beyond. It also is the home of the state’s only National Cancer Institute (NCI)-designated Comprehensive Cancer Center, a Level IV Neonatal Intensive Care Unit that cares for the tiniest and sickest newborns, the region’s only Level 1 trauma center and Kentucky’s top hospital ranked by U.S. News & World Report.
As an academic research institution, we are continuously pursuing the next generation of cures, treatments, protocols and policies. Our discoveries have the potential to change what’s medically possible within our lifetimes. Our educators and thought leaders are transforming the health care landscape as our six health professions colleges teach the next generation of doctors, nurses, pharmacists and other health care professionals, spreading the highest standards of care. UK HealthCare is the power of advanced medicine committed to creating a healthier Kentucky, now and for generations to come.