Two families, one mission: turning NICU stories into lifelines for others
LEXINGTON, Ky. (Sept. 25, 2025) — It’s a place that can feel overwhelming from the moment you step inside — an atmosphere of blinking lights, constant beeps and urgent footsteps. Even the name is harrowing: the neonatal intensive care unit (NICU). Families spend months dreaming of the day they bring their new baby home, only to be faced with unexpected detours into a world of beeping monitors and urgent care.
But inside, it’s a place filled with hope, love and support. Families facing the worst days of their lives are lifted — emotionally and sometimes physically — by a compassionate team of nurses, physicians, social workers, respiratory therapists, pastoral staff and more, dedicated to providing expert care to the tiniest of patients.
For some families, the NICU is the start of a lifelong story. For others, it holds their final, most precious moments. In both joy and loss, the bonds formed here endure — and inspire. Two families, whose journeys ended in very different ways, chose to honor their babies by supporting other families and patients across the children’s hospital.
Blake’s story
On Jan. 8, 2018, Blake Russell made his world debut, albeit unexpectedly. His mother Elizabeth Clevinger said he loved music, being held and visits from his favorite NICU nurses. Blake lived all 209 of his days in the hospital, but every one of those days was filled with tenderness and love.
Blake came to the NICU at Kentucky Children’s Hospital (KCH) on his second day of life; it was another two days before he and Elizabeth were reunited.
“I was tired, scared, overwhelmed, confused and still in a lot of physical pain myself,” Elizabeth said. She was met by a nurse named Alice who would go on to become a close friend. “She helped me to our baby, explained to me what every wire and monitor meant, and assured me that she had taken care of countless babies in her 30-year career. I remember absolutely nothing that she told me that day, but I do remember being so comforted by the fact someone so amazing was taking care of our baby and hoping she would be there every day.”
Over the next six months, Alice, another nurse named Nikki, along with countless other nurses and NICU staff members made indelible impressions on Elizabeth, Blake’s dad Anthony and her family. They would come in to find that Blake’s bed would magically have new, cozy sheets. Major milestones such as his first bath and first Down Syndrome Awareness Day were widely celebrated. Alice and Nikki would come in on their days off, stay past their shifts or come in early just to check on Blake. They advocated on Elizabeth and Anthony’s behalf, insisting on further testing and more opportunities for Blake to be held. They also assured them that it was ok to leave the hospital and take a break.
On March 21, Blake’s 73rd day of life, he underwent major heart surgery. Alice was there at every moment; holding Elizabeth’s hand as he was taken to the operating room, taking her to meet the nurses who would be caring for him after his procedure, checking on her in the waiting room and meeting with the surgeons afterward to help her understand everything that happened.
Beyond their duties as healthcare providers, Elizabeth noted how each NICU staff member seemed perfectly attuned to families’ needs. Blake was dressed each morning in special onesies that accommodated his gastrostomy tube, in a bed with adorable sheets and a matching blanket; none of which were standard hospital issue, but instead gifts from the NICU caregivers. With gratitude — and a pang of guilt — she realized these gifts were funded by the nurses themselves.
“We had some lovely nurses who would do these things for us, and I know for a fact that they were paying for it out of pocket,” she said. “The gestures meant so much, but I don’t want the nurses to use their own money to pay for that stuff.”
On Aug. 4, Nikki and Alice stepped up again, this time to help Elizabeth, Anthony and their family grapple with the anguish of Blake’s passing. The kindness and compassion they and the NICU staff showed through this agonizing time is something Elizabeth will never forget and feels she can never repay. Determined to support other families in the way she had been, she set about collecting the small comforts she knew would help others.
On what would have been Blake’s first birthday, Elizabeth called her NICU nurse friends and asked what families needed. Then she went shopping. It became a tradition, spending what she would have spent on Blake’s birthdays on gifts and necessities for NICU families — gift cards for meals and gas, wagons, clothes and blankets. After five years of honoring Blake’s birthdays this way, Elizabeth decided she wanted to create something more sustainable to help NICU families for years to come. While serving on the NICU Parent and Family Advisory Council, she had the idea to start the Blake Stephen Russell Endowed Fund for NICU Families, a pool of donated funds that can be used to provide for support for any NICU patients, such as adaptive onesies that fit around g-tubes or wagons to carry supplies for patients with complex care needs, as well as small comforts such as toys and Starbucks gift cards.
“There’s a need for big problems, such as housing, food and accommodations, but there’s also a need for small problems,” Elizabeth said. “And I hope this can fill this gap. It’s about making things easier for families. I want this to help as many people as possible while also saying thank you.”
In addition to monetary support, Elizabeth serves as a peer mentor for NICU families, helping them navigate the complexities of critical care while also being a shoulder for those struggling with the emotional weight that comes with a prolonged NICU stay.
“It could be a day, a week or it could be a year,” she said. “But no matter what it looks like, they aren’t alone, and there’s someone who’s walked the road ahead of them. As parents who went through it, we wished we had someone tell us it was ok to go home and sleep, take your other kids to church or whatever they need to do. There’s a connection between that and the funds. Those things sound really small, but when you’re faced with some really challenging things, those small things can make a big difference.”
Henry’s story
Kelli Romond was in the homestretch of an uneventful pregnancy. She and her husband John had their hospital bags packed and ready and were counting down the days until they were parents.
A week before her due date, at 1:20 a.m., Kelli woke John up, telling him her water broke and that it was time to go. When she went to the bathroom and turned on the light, she was horrified to discover that what she felt wasn’t her water breaking — she was hemorrhaging blood.
John recalls they made the two-mile drive to the University of Kentucky Albert B. Chandler Hospital in record time. But he says what happened next was the perfect confluence of serendipitous events that made survival possible against all odds.
“There are things that my mom refers to as a moment of grace, where the universe conspires in your favor,” John said. “From the moment Kelli went back, for as horrific as an experience as it was, everything that could have gone wrong went right.”
The first was that the obstetrician who happened to be on duty that night had just finished a fellowship in high-risk pregnancies. During the ultrasound, she noted that the baby’s heartrate was slow and weak, necessitating an emergency C-section. After Kelli was wheeled into the operating room, John, then a resident doctor at Chandler Hospital, used his badge access to watch from an adjacent room. He almost wished he hadn’t.
“Henry was limp and lifeless,” said John. “He didn’t have a heartbeat, was gray and not moving at all.”
Next came the second occurrence of cosmic happenstances. Neonatologist Sumit Dang, M.D., was on duty in the NICU, and not in India at his brother’s wedding as he was originally scheduled to be. He was first on the scene, ‘running a code,’ hospital shorthand for an urgent, all-hands-on-deck effort to save a life. After 10 minutes, the universe delivered the third fortuitous occurrence: attending physician Hubert Ballard, M.D., who also wasn’t scheduled to work that night. While covering for another physician, he heard the call that a newborn baby was crashing. He rushed to the operating room, and saw John, a friend and colleague, ashen face at the sight of his lifeless newborn son. Ballard joined Dang, performing CPR on little Henry for another eight minutes, intuitively knowing there was a spark of life in there. Finally, there was a heartbeat. As Henry was taken to the NICU and Kelli was moved to a recovery room, Ballard stopped to give John a report.
“John, he’s a redhead.”
But Henry wasn’t out of the woods; 18 minutes is a long time to go without a heartbeat. With their medical training, John and Kelli knew what happens when the brain goes without oxygen for 18 minutes, and prepared themselves to bring home a baby with significant developmental and physical impairments.
“I have this memory of hoping and praying Henry had enough brain to know that he was loved,” John said. “If his kidneys didn’t work, we’d take him to dialysis. If his liver shut down, we’d figure it out. If he had trouble breathing, we would still hold him. But I wanted him to have enough brain to know we loved him.”
Maintaining body temperature is critical for babies as fragile as Henry. With a heartbeat established, Dang, knowing the danger of warming Henry’s little body too quickly, turned off the heat lamp. For three days, under the watchful eye of the NICU staff, Henry’s body was cooled, then warmed very slowly to reduce the risk of dangerous heart rhythms and seizures. Finally, after days of agonizing watching and waiting, Henry opened his eyes and John and Kelli finally got to hold him. On day seven, Henry had an MRI to assess the extent of the damage to his brain.
There was no damage; the MRI showed no abnormalities.
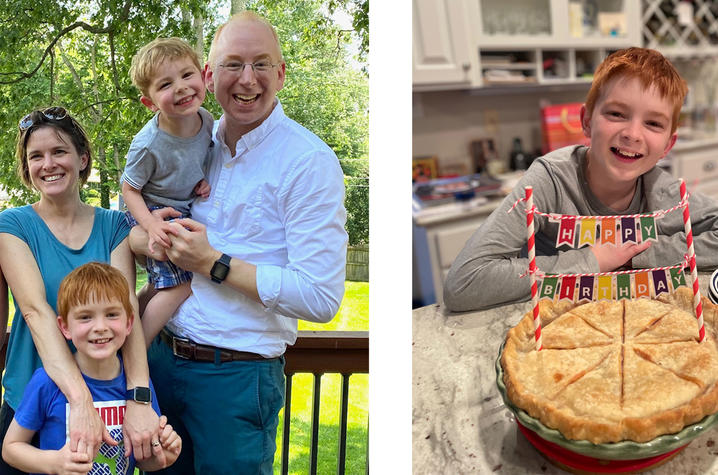
After 11 days in the NICU, John and Kelli, still in disbelief at the incredible confluence of coincidences, brought Henry home. That was 12 years ago; Henry is now a bright and inquisitive seventh grader who loves soccer, video games and his younger brother Charlie. He made the academic team at his school and can solve a Rubik’s cube in record time. Though he’s now entering his period of middle school angst, the Romonds remind themselves that these are exactly the kinds of problems they were hoping for.
While it seems like the stars all aligned for the Henry, the Romonds know the real magic is the expertise and compassion of UK HealthCare providers.
“If we were somewhere else, Henry would have died,” said Kelli.
Henry knows a little about his dramatic entrance to the world. But he knows even more about the gratitude his family has for the expert care of the physicians, nurses and staff of the NICU. The Romonds remain close with Ballard, Deng and all the others to thank them for their quick thinking and even quicker action. Like fellow NICU mom Elizabeth Clevinger, they too wanted to have a bigger, more substantial impact to give back to the people who helped them so much. After conferring with UK Philanthropy, Kelli and John made a gift to the Rupp Family Endowed Fund for Pediatric Psychology, a fund that provides wraparound psychosocial support to the families in the NICU and neonatal abstinence care unit (NACU).
“Having a baby in the NICU can be an incredibly stressful experience for all family members,” said Meghan L. Marsac, KCH pyschologist and chief of the Division of Psychology in the UK College of Medicine. “Here at UK HealthCare, we are doing everything we can to provide the best care possible for our patients as well as their families. Providing mental health and psychosocial support for patients and their families is an essential part of healthcare. We are very grateful for the donation provided by the Romonds. With their help, we can extend our ability to provide psychosocial support to more NICU families and train mental health professionals to specialize in NICU care. The generosity of the Romonds will help us support other families as they navigate through their NICU journeys.”
“We will always, always be grateful to UK,” said Kelli. “And we have told them many times that we will never be able to pay them back.”
***
The NICU is a place where life’s most fragile moments unfold. For Elizabeth Clevinger and the Romonds, those moments sparked a lasting commitment to help others navigate the road they traveled. Health care providers deliver expert medical care, but fellow families can bring the comfort and connection that make the journey a little easier. In honoring their own children’s stories, they are helping write new ones for countless families yet to come.
UK HealthCare is the hospitals and clinics of the University of Kentucky. But it is so much more. It is more than 10,000 dedicated health care professionals committed to providing advanced subspecialty care for the most critically injured and ill patients from the Commonwealth and beyond. It also is the home of the state’s only National Cancer Institute (NCI)-designated Comprehensive Cancer Center, a Level IV Neonatal Intensive Care Unit that cares for the tiniest and sickest newborns and the region’s only Level 1 trauma center.
As an academic research institution, we are continuously pursuing the next generation of cures, treatments, protocols and policies. Our discoveries have the potential to change what’s medically possible within our lifetimes. Our educators and thought leaders are transforming the health care landscape as our six health professions colleges teach the next generation of doctors, nurses, pharmacists and other health care professionals, spreading the highest standards of care. UK HealthCare is the power of advanced medicine committed to creating a healthier Kentucky, now and for generations to come.