KCH clinic builds powerful community for patients with sickle cell disease
LEXINGTON, Ky. (Sept. 18, 2025) — Imagine that one day, out of the blue, you are gripped by the most unimaginable, debilitating pain. It’s a pain that’s been described as burning or stabbing, and it’s all over your body — no pain reliever can touch it. The pain can last hours, days or weeks. And it comes on without any warning.
That’s the silent threat faced by the approximately 80 patients with sickle cell disease (SCD) who are treated in the DanceBlue Kentucky Children’s Hospital Hematology/Oncology Clinic. But those patients have a powerful ally against that ever-looming threat: the dedicated staff of the Sickle Cell Clinic.
Sickle cell disease, is an inherited hemoglobin-related blood disorder. Sickle shaped red blood cells have a shortened lifespan but they also don’t flow as smoothly through the blood vessels as the round ones, which results in the blood flow being blocked. These two processes, the breakdown of the red blood cells and obstruction of small vessels, account for the pain crisis but also for the progressive damage to the internal organs. People with sickle cell disease are predicted to have a life-expectancy 15-20 years shorter than the general population
“Sickle cell disease is a lifelong, chronic, debilitating condition,” said Vlad Radulescu, M.D., medical director for pediatric hematology and oncology at Kentucky Children’s Hospital (KCH) and primary hematologist for the sickle cell clinic. “The most effective interventions are preventative: we try to anticipate complications before they clinically manifest and intervene.”
Preventative treatments include immunizations, prophylactic antibiotics, aggressive management of infections and tests to identify patients at risk of stroke, gallstones, heart or kidney complications. Aside from the debilitating pain, patients who experience sickle cell crises are at risk for severe complications such as severe infection and acute chest syndrome, the leading cause of hospitalization of sickle cell patients in which oxygen levels drop and abnormal substances accumulate in the lungs. Stroke and splenic sequestration — a condition in which blood cells become trapped in the spleen, causing it to enlarge — are other threats faced by those with sickle cell disease.
Severe pain. Stroke. Permanent organ damage. All potentially caused by a disease that’s considered invisible because the symptoms can only be felt, not seen. And it’s happening to a child.
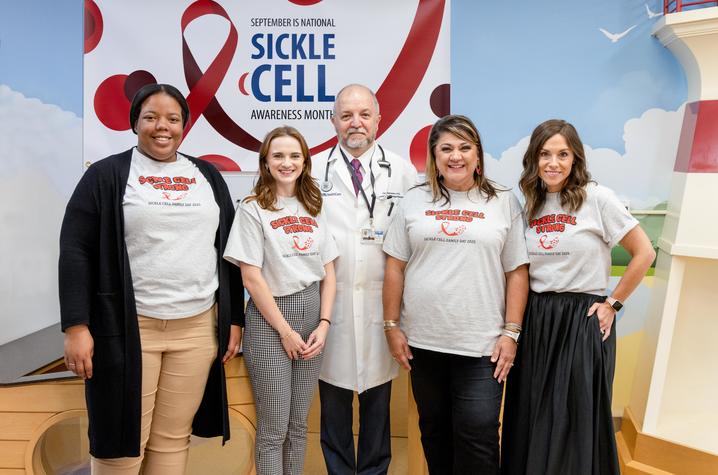
It can be incredibly isolating and overwhelming for a family to navigate this diagnosis, and parents feel helpless when watching their child in the throes of a brutal fight against an invisible enemy. But at KCH, there is team that fights just for them: Radulescu as the primary physician, nurse navigator Crystal Aukerman, nurse practitioner Andrea Haggard, social worker Meridith Kress, psychologist Tanesha Johnson and school interventionalist Rachael Seals. Together, they provide not just medical treatment, but complete, all-encompassing support for the patient’s whole family.
On the medical side, there’s the preventative and maintenance: genetic counseling for newborn screens, medication management, personalized pain plans, blood transfusions and red blood cell exchanges and lab monitoring. Along with specialists in other areas, they provide routine monitoring to help prevent sickle related complications, such assessing stroke risk, hearing and vision screenings, abdominal ultrasounds, MRIs of the head, heart and liver, lung function testing, echocardiograms and neurocognitive testing for school-age children. Recently, the clinic became a member of the National Alliance of Sickle Cell Centers (NASCC) and adheres to standardized guidelines.
“When I started, we had about 20 patients with sickle cell disease,” said Radulescu, who came to KCH in 2006. “I became their primary hematologist, at the time we shared a nurse navigator with pediatric oncology, and we used one of the two social workers who supported the division. We have grown quite a bit; we see 80-90 patients and have a full team dedicated to these patients.”
“The biggest thing that makes us stand out to help care for our sickle cell warriors and their families is our amazing team,” said Aukerman. “Some of our patients are seen on a monthly basis for chronic blood transfusions or red blood cell exchanges, some are followed every six to 12 weeks for medication management and lab monitoring and some are followed on a yearly basis. Our treatment plans are dependent on the type of sickle cell disease the patient has, and their supportive needs.”
That support doesn’t stop at the clinic door. Social worker Meridith Kress recognizes the toll sickle cell disease can take on the whole family. For example, parents have to miss work or can’t find childcare for their other children. Several SCD patients and families don’t speak English and require an interpreter. Even just getting to Lexington for treatment or hospital stays can be a burden. Kress connects them with resources for transportation, financial assistance, as well as connecting families to regional and national organizations for sickle cell disease.
“As the social worker for our sickle cell patients my role is to support the patient and family throughout their treatment both inpatient and outpatient and address any barriers to care there may be,” said Kress. “Our patients can face a lot of hardship within the medical system and elsewhere due to various possible factors such as racial discrimination, language barriers, socioeconomic status, cultural differences and their illness often being an invisible one. I believe our treatment team here has done a fantastic job at recognizing that psychosocial stressors can have just as much if not more of an impact on a patient’s wellbeing as the disease itself.”
Then there is school — a kid’s only job other than just being a kid. Because of rigorous preventative treatment protocol, as well as the disease’s unpredictable nature, it can throw a patient’s attendance in school or their ability to stay on top of their workload into turmoil. As the clinic’s dedicated school intervention specialist in the PAWS program, Rachael Seals serves as an advocate for the patients at the school, assisting with establishing individual health accommodation plans that address both attendance challenges and medical needs.
“I focus on maintaining strong relationships with school teams through consistent communication while also providing recommendations, in-service education, and resources that help empower school staff and students stay connected and engaged despite the complications of SCD,” said Seals. SCD isn’t a rare disease, but it is not one many people know about. By educating teachers, school administrators and even the patient’s classmates, Seals helps build a supportive, accommodating learning environment to help keep the patient on track.
So while Radulescu and Haggard attend to the patient’s medical needs, Aukerman serving as the nurse navigator, helping families chart a course through the often confusing medical system, Kress helping with the social support and Seals working with schools, there is another team member who is the final piece of the puzzle, completing the picture of the patient’s overall physical, social and emotional wellbeing.
“For some patients, having SCD can be an isolating experience,” said pediatric psychologist Tanesha Johnson, Ph.D. “Loss or disruption of normal childhood activities for children with sickle cell disease often is associated with children and their families feeling distressed, disappointed and/or anxious about the future. Due to the chronic health impact of sickle cell disease, our patients are at higher risk to developing anxiety and depression.”
As the dedicated psychologist, Johnson, ensures that patients can be seen for therapy as part of their medical visit. Using evidence-based practices, patients are equipped with coping strategies the stress associated with experiencing chronic pain, how to manage living with SCD as part of their lives, providing education about the interaction between pain and stress, as well as any other mental or emotional concerns the patient might have.
“For some patients, having SCD can be an isolating experience,” Johnson said “Due to not knowing other people with SCD and not wanting to be different from their peers by hiding their disease, they often struggle with maintaining friendships.”
But this team knows there is strength in numbers. And with a sizable pediatric population with SCD, the clinic staff know a strong community can help patients and their families in ways they can’t. Recently, they hosted the second annual Sickle Cell Family Day at Evan’s Orchard in nearby Georgetown, bringing together the patients and families and showing them that when faced with a serious chronic disease, no family has to fight alone.
“We first started the event to help create a space outside of the clinical setting for families to connect and receive educational resources pertinent to their disease management,” said Haggard. “Another reason we wanted to start this annual event is because we would often hear from many of our patients that they have never met another person with sickle cell. We want to help create a community for our warriors that empowers self-advocacy and helps build sickle cell awareness by providing information that is relevant and transformational to their health.”
This dedicated staff of providers fights for their patients. They are constantly exploring new treatments options to help their patients live without pain or risk of severe complications.
“We are working to pursue the only curative options currently available for sickle cell disease bone marrow transplant and gene therapy,” said Radulescu. “We currently have several patients in different stages of evaluation for and treatment with gene therapy. “
As Radulescu and his team advocate for their patients, they are always looking for ways to expand their array of supportive resources, as well as their physical clinical space as their patient population increases. But for now, as their patients grow up and transition to adult care, the staff know they will leave their clinic with knowledge, self-advocacy and coping skills needed to manage their lifelong condition.
“We are committed to setting our patients up for success when they transition out of pediatrics,” said Radulescu. “Sickle cell is tough, but so are our patients, and we stand beside them.”
September is National Sickle Cell Awareness Month, designated by Congress to help focus attention on the need for research and treatment of sickle cell disease. Find more information and resources here.
UK HealthCare is the hospitals and clinics of the University of Kentucky. But it is so much more. It is more than 10,000 dedicated health care professionals committed to providing advanced subspecialty care for the most critically injured and ill patients from the Commonwealth and beyond. It also is the home of the state’s only National Cancer Institute (NCI)-designated Comprehensive Cancer Center, a Level IV Neonatal Intensive Care Unit that cares for the tiniest and sickest newborns and the region’s only Level 1 trauma center.
As an academic research institution, we are continuously pursuing the next generation of cures, treatments, protocols and policies. Our discoveries have the potential to change what’s medically possible within our lifetimes. Our educators and thought leaders are transforming the health care landscape as our six health professions colleges teach the next generation of doctors, nurses, pharmacists and other health care professionals, spreading the highest standards of care. UK HealthCare is the power of advanced medicine committed to creating a healthier Kentucky, now and for generations to come.