Markey researchers identify genetic marker that could guide brain cancer treatment
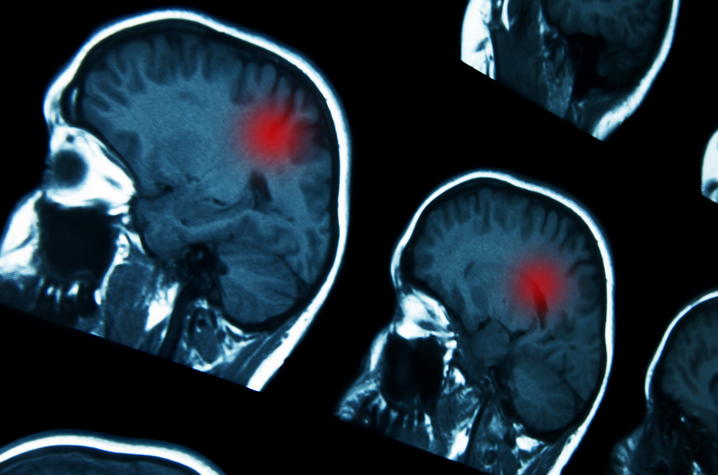
LEXINGTON, Ky. (July 25, 2025) — University of Kentucky Markey Cancer Center researchers have discovered a genetic biomarker that could help identify patients with glioblastoma most likely to benefit from the cancer drug bevacizumab.
The study, published in JCO Precision Oncology, found that brain tumors from patients treated with bevacizumab who lived longer were more likely to have a genetic change called CDK4 amplification. This suggests that testing for the molecular marker could help oncologists identify patients most likely to respond well to bevacizumab treatment.
“The findings could help oncologists make more informed treatment decisions for glioblastoma patients, potentially sparing those unlikely to benefit from unnecessary side effects while ensuring those who might respond get access to the drug,” said John Villano, M.D., Ph.D., the study’s lead author and professor in the UK College of Medicine.
Glioblastoma accounts for about 15% of all brain tumors and usually occurs in adults between the ages of 45 and 70. It is the most aggressive form of brain cancer, with patients typically surviving less than 15 months following diagnosis.
Bevacizumab, one of the medications commonly used to treat recurrent glioblastoma, works by blocking blood vessel growth in tumors. For many patients, its use has been associated with increased progression-free survival and improvement in symptoms and quality of life. However, there has been no way to predict patients that would benefit the most from the treatment.
The research team analyzed tumor samples from 3,106 glioblastoma patients, including 571 who received bevacizumab. Using next generation sequencing data, they compared the molecular profiles of patients who stayed on treatment for different lengths of time.
This research represents the first large-scale study to identify molecular markers associated with prolonged bevacizumab response in brain cancer patients.
The study’s collaborators include UK faculty members Catherine Garcia, M.D.; Rachael Morgan, Pharm.D.; Farhan Mirza, M.D.; and Shulin Zhang, M.D. The team also included Jill Kolesar, Pharm.D., former director of Markey’s Precision Medicine Clinic and current dean at the University of Iowa College of Pharmacy.
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number P30CA177558. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
UK HealthCare is the hospitals and clinics of the University of Kentucky. But it is so much more. It is more than 10,000 dedicated health care professionals committed to providing advanced subspecialty care for the most critically injured and ill patients from the Commonwealth and beyond. It also is the home of the state’s only National Cancer Institute (NCI)-designated Comprehensive Cancer Center, a Level IV Neonatal Intensive Care Unit that cares for the tiniest and sickest newborns and the region’s only Level 1 trauma center.
As an academic research institution, we are continuously pursuing the next generation of cures, treatments, protocols and policies. Our discoveries have the potential to change what’s medically possible within our lifetimes. Our educators and thought leaders are transforming the health care landscape as our six health professions colleges teach the next generation of doctors, nurses, pharmacists and other health care professionals, spreading the highest standards of care. UK HealthCare is the power of advanced medicine committed to creating a healthier Kentucky, now and for generations to come.




