Teacher and UK Patient Back in the Classroom After Dual-Organ Transplant
LEXINGTON, Ky. (Sept. 9, 2013) – After 34 years of teaching, many schoolteachers would be ready to retire or move on to new things.
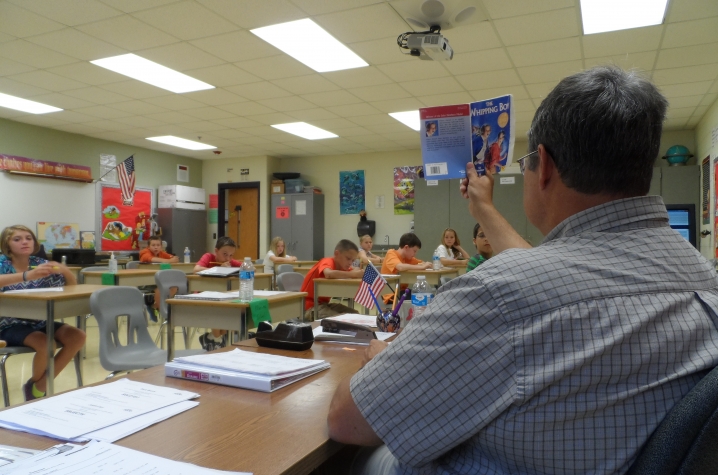
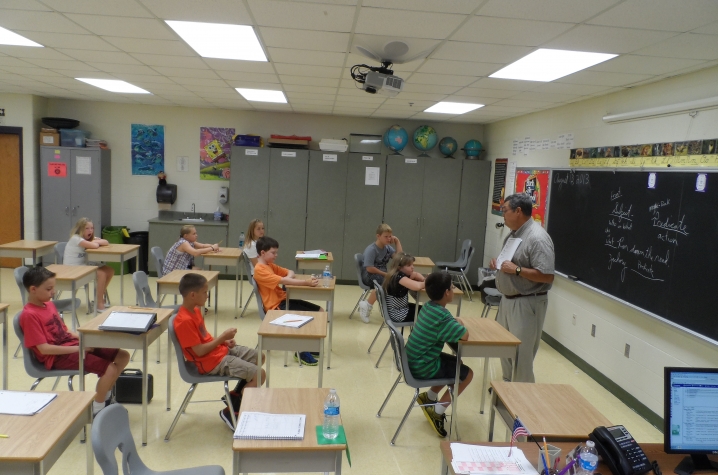
Not David Morrow. The 57-year-old science and language arts teacher at East Washington Middle School in Pekin, Ind., is now in his 35th year of teaching and still going strong.
That alone is impressive enough. Even more impressive? The fact that Morrow is back in his classroom today after undergoing a combined heart and kidney transplant at UK Chandler Hospital last November.
But for those who know Morrow best, his determination comes as no surprise.
“He’s probably one of the most stubborn men you’ll ever meet,” said Linda Leudeman, former principal at EWMS who has known David for nearly 15 years. “Which is probably a big reason why he’s here today, because he did not give up.”
Morrow’s health troubles had been going on for some time. Six years ago, he was diagnosed with congestive heart failure and received an internal cardiodefibrillator (ICD). Then his kidneys began to shut down, and Morrow began receiving dialysis under the care of Dr. Jayakrishnakamal Konijeti of Nephrology Associates of Kentuckiana (NAK).
However, despite these measures, his health continued to deteriorate. Morrow’s NAK doctors then referred him for a kidney transplant. After an initial meeting with the transplant team at UK’s Transplant and Specialty Clinic at Norton Audubon Hospital in Louisville, David met with Dr. Navin Rajagopalan, UK’s medical director of cardiac transplantation, and got some surprising news.
“He said, we can’t just give you a kidney by itself, because we don’t think that is the major issue, we think it’s your heart,” Morrow said. “So he said, what we can do is a heart and a kidney transplant.”
End-stage kidney disease is a contraindication for a heart transplant – if the kidneys are not working, it puts a much greater strain on the heart, and a patient in this condition who receives a heart transplant will face a tough road to recovery – and will likely end up with the same heart failure as before.
However, for patients who have both heart and kidney failure, combined dual-organ transplants offer a better chance for survival. Because of the amount of resources and expertise required for the procedure, the combined transplants are not very common, according to Rajagopalan.
“A lot of centers don’t consider patients for dual-organ transplant, and there are not many heart/kidney transplants performed each year,” Rajagopalan said. “But David was the perfect individual for a combined heart/kidney transplant. He is diabetic, but otherwise reasonably healthy. And he was very motivated.”
Konijeti, who also serves as chief of staff at Floyd Memorial Hospital in New Albany, In., says Morrow was referred to UK because of the complexity of his case.
“We knew there was going to be issues because of his heart failure,” Konijeti said. “So it wasn’t just a matter of getting a kidney, because the new kidney would have the same problem. We needed to send him to a place that had the appropriate expertise and experience to be able to evaluate him from both a combined heart and kidney transplant.”
Initially, Morrow said he had reservations about undergoing such a major procedure.
“I wasn’t too worried about the kidney – I knew I could live without that, going on dialysis, but when he said the heart transplant, I had to think,” Morrow said. “But I just kept getting worse and worse, and I told my wife, ‘I’m not going on like this, I’m doing to do something about it.’”
Morrow began the process of evaluation for transplant. He underwent rounds of testing, and throughout the spring of 2012, was in and out of the hospital with a variety of problems. Then, two weeks before the school year was up, Rajagopalan told Morrow he needed to be admitted to the hospital – and this time, he would be staying indefinitely.
Always thinking of his students, Morrow protested at first. He only had two weeks left – he needed to wrap up the school year, get his final grades posted.
“So we bought a laptop computer, and I was down there at UK punching grades in,” Morrow said. “But by the end of school, I was ready to go. I was leaning against the wall, out of breath, not able to walk 30-40 feet.”
Morrow was admitted to UK Chandler Hospital on May 31, 2012. However, his heart failure continued to worsen and he became weaker and weaker. He had to be taken off the transplant list, as he was too weak to survive such a major operation should the organs even become available.
“My heart kept deteriorating,” Morrow said. “I was probably at UK for about 2-3 weeks, and I was sitting in bed with one of the ICU nurses one day and she shouted ‘We have a V-tach!’ I looked around and said, ‘Who is it?’ and she said, ‘it’s you.’”
Morrow was so sick, he required “double bridge” to transplant – he first received extracorporeal membrane oxygenation (ECMO) treatment to stabilize his condition. Then, he received both a right and left ventricular assist device (known as a BVAD) to perform the work of his failing heart. With the assistance of these technologies – and the constant support of his friends, family, and medical team – his health began to improve. He got up out of bed and walked laps around the ICU to gain back his strength. He became strong enough to get reactivated on the transplant list.
Morrow’s quick recovery and improvements following the BVAD surgery even surprised his doctors.
“I was actually on vacation and I got an email that he’d been reactivated,” Rajagopalan said. “I said, already? And my Transplant Coordinator Donna Dennis said, yeah, he looks great. He’s walking, taking laps around the ICU. He’s ready to be listed.”
And as his cardiac health improved, his kidneys even began functioning on their own.
“I improved so much my kidneys started working again,” Morrow said. “I didn’t have to do dialysis, which was great. That was a plus, and that kind of encouraged me and lifted my spirits.”
His health had improved drastically, but the BVAD required that Morrow remain in the hospital until his transplant. And although his kidney function had improved, they remained marginal and he still needed a new kidney along with the heart. After getting reactivated on the transplant list, all that was left for him to do was wait.
It took more than five months. But on Nov. 5, 2012, Morrow got the news he’d been waiting for. Led by UK transplant surgeons Dr. Charles Hoopes and Dr. Roberto Gedaly, Morrow underwent surgery to receive his new heart and kidney. A month later, he went home – just in time for the holidays.
Over the next few months, Morrow came back to the hospital a few times to address some minor complications from surgery. But after a few bumps in the road to recovery, he continued to grow stronger and healthier. He made plans to go back to the job he loved.
While some of Morrow’s colleagues were shocked to see him returning to the classroom so quickly, Leudeman – who visited Morrow several times during his stay at UK – said she wasn’t surprised at his determination to come back.
“He always said he wanted to come back, and I tried to talk to him about that,” Leudeman said. “But he knew he wanted to be here with the kids. That was his priority. That was his focus.”
A patient’s attitude plays a critical role both pre- and post-surgery, says Rajagopalan, and Morrow’s resolve only reinforced why he was the perfect candidate for the dual-organ transplant in the first place.
“The way I look at it, David was teaching even while he was on dialysis and had a weak heart, so why shouldn’t he teach now?” Rajagopalan said. “The fact that he continued to teach school while on dialysis really showed how dedicated and motivated he was, so we knew he would be an excellent transplant candidate. Donors rely on us to make sure their gift will be well taken care of. Patients need to be medically good candidates, but also good candidates that will take care of their organs. And we knew that was the case with David.”
Morrow officially started back at EWMS in August. He continues to receive follow-up care close to home from both his physicians at NAK and Rajagopalan at the UK Transplant Clinic in Louisville. And as he embarks on his 35th year of teaching, he says he’s glad to be back – and plans to be back for some time to come.
“It gives me purpose, I guess you might say,” Morrow said. “I enjoy it. A lot of these children come in, and their parents were in my classroom. I told them, when they start getting the grandchildren in here, then I believe it’s time for me to step down.”
*****
An average of 18 people die every day in the U.S. waiting for an organ transplant and more than 113,000 men, women and children are on the national waiting list. A new name is added to the waiting list every 11 minutes.
The best way to honor those who gave the ultimate gift of life and to celebrate the new life of transplant recipients is to register on the Kentucky Organ Donor Registry. The registry is a safe and secure electronic database where a person’s wishes regarding donation will be carried out as requested.
To join the registry, visit www.donatelifeky.org or sign up when you renew your driver’s license. The donor registry enables family members to know that you chose to save and enhance lives through donation. Kentucky’s “First Person Consent” laws mean that the wishes of an individual on the registry will be carried out as requested.
MEDIA CONTACT: Allison Perry, (859) 323-2399 or allison.perry@uky.edu