Full-court press against Parkinson’s: Former Texas A&M Coach Billy Kennedy finds hope at UK
LEXINGTON, Ky. (March 17, 2025) — As March Madness sweeps the nation and college basketball takes center stage, a former coach’s journey off the court is proving just as inspiring as any Cinderella story on the hardwood.
Billy Kennedy, former head coach of Texas A&M, has spent his career developing game plans, mentoring players, and leading teams through the highs and lows of competition. But in 2011, he faced an unexpected opponent — Parkinson’s disease.
For Kennedy, the diagnosis was a game-changer, but not a game-ender. His fight against the disease, much like his coaching career, has been defined by resilience, strategy and faith.
Thanks to innovative research at the University of Kentucky, Kennedy has not only maintained a high quality of life but has also played a crucial role in shaping the future of Parkinson’s treatment. His participation in the DBS-Plus study — an experimental procedure combining deep brain stimulation (DBS) with an additional nerve graft — has provided researchers with invaluable data.
Now, that research is leading to the next phase of innovation: the LEAP trial, which aims to intervene earlier in Parkinson’s progression.
The first half: A Parkinson’s diagnosis
Kennedy was at the height of his coaching career in 2011, having just moved to College Station to take over as Texas A&M’s head coach after five seasons at the helm for Murray State University. But something wasn’t right. A nagging stiffness in his neck wouldn’t go away, and eventually, doctors confirmed what no coach wants to hear — his body was working against him. Parkinson’s, a progressive neurological disorder, would inevitably impact his movement, speech and daily activities.
Like many newly diagnosed patients, Kennedy turned to the internet, searching for answers.
“When I was first diagnosed, I read things I shouldn’t have read,” he recalls. “It was very negative. But my life hasn’t turned out that way. I’ve been blessed.”
Despite the diagnosis, Kennedy pressed forward, continuing to coach and recruit at a high level. He adapted, just as any great coach would when facing a tough opponent. He remained committed to his team, his faith and his family.
The assist that changed the game
Three years after his diagnosis, a friend with connections to Kentucky and Texas, urged Kennedy to consider an experimental study at UK — DBS-Plus, an innovative approach to Parkinson’s treatment and a first-of-its-kind clinical study aimed at stopping or reversing the degenerative effects of the disease. It’s supported by a $3.3 million, five-year grant from the National Institutes of Health and builds on research supported by the UK Center for Clinical and Translational Science’s pilot program funding.
Since the early 1900s, scientists have known that peripheral nerves, which exist outside the brain and spinal cord, possess regenerative qualities that central nervous system nerves do not. The team at UK is hopeful they can leverage those regenerative effects within the brain, potentially halting or reversing nerve damage caused by Parkinson’s.
“While the peripheral nervous system can repair itself, the central nervous system does not do a very good job of it,” said UK’s chair of neurosurgery, Craig van Horne, M.D., Ph.D., the study’s principal investigator. “So, the question is: Can we tap into the ability of the peripheral nervous system’s response for repair? Can we bring that to the central nervous system?”
At first, Kennedy hesitated. He felt he was managing his symptoms well enough with medication. But his friend was persistent. He arranged for Kennedy to visit the research team at UK, even offering him a place to stay while in town.
After touring the facility and meeting with van Horne, Kennedy felt comfortable enough to take the next step. He enrolled in the DBS-Plus study, undergoing the first phase of the procedure in 2015. The surgery involved taking a nerve graft from his ankle and implanting it in his brain along with the standard deep brain stimulation treatment.
The results were remarkable. Kennedy noticed a significant reduction in his need for medication. His symptoms stabilized, and the dyskinesia (uncontrollable movements caused by Parkinson’s medication) disappeared.
“I can do anything I’ve always done,” he says. “Exercise-wise, career-wise — it’s helped me all the way through.”
Still in the game
Many might have assumed Kennedy would step away from basketball after his diagnosis. But stepping away was never in his game plan. Even after undergoing surgery, he continued to coach — making multiple post season runs, including to two NCAA Sweet Sixteens. Still today, after closing out his coaching career he remains involved in basketball, moving into a scouting role for the NBA’s Oklahoma City Thunder.
Kennedy’ routine remains rigorous. He jogs, lifts weights, plays pickleball and even hits the tennis court occasionally.
“Exercise is key,” he said, acknowledging its benefits in managing Parkinson’s. “It’s a good remedy.”
His only noticeable symptom? A softer voice.
“I was never that loud to begin with,” he joked, “but my voice has declined some.”
Despite that, his impact in the basketball world and in the Parkinson’s community remains as strong as ever.
A full-circle moment in Lexington
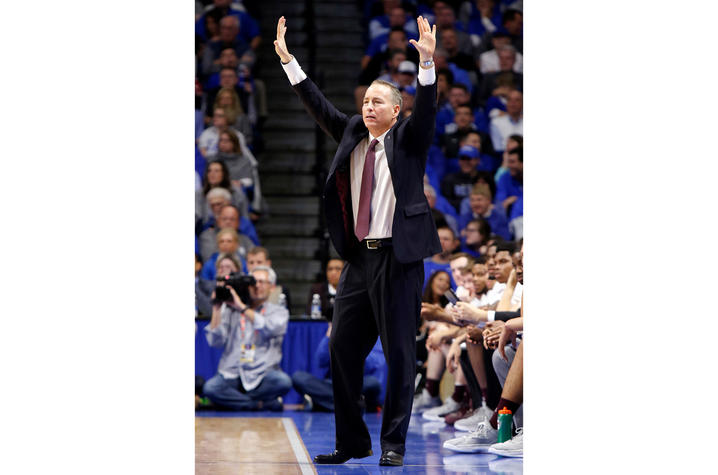
For much of his coaching career, Lexington, Kentucky, was enemy territory. Some of the more memorable moments during Kennedy’s run as the Aggies head coach feature UK. That includes leading A&M to their first conference title in 30 years when they shared the SEC crown with Kentucky for the 2015-16 season. They also made the SEC tournament final that season before losing to Kentucky in overtime.
As the head coach of Texas A&M, he faced off numerous times against the Wildcats in their home at Rupp Arena, one of college basketball’s most intimidating venues.
“It wasn’t always the friendliest place for me,” Kennedy said with a laugh.
Now, Lexington represents something entirely different — a place of healing, progress and gratitude. He returns to UK periodically for adjustments to his DBS device, working with a team that has become an integral part of his journey.
“I’m incredibly grateful for the care and research here,” he said.
The LEAP trial: Advancing Parkinson’s research
Kennedy’s participation in the DBS-Plus study, along with other dedicated patients, has provided researchers with the data they needed to push forward. Now, the University of Kentucky is launching its most ambitious Parkinson’s trial yet—the LEAP trial.
This is all thanks to the work done thus far in the DBS studies, including one known as the STAR trial. Greg Gerhardt, Ph.D., John Slevin, M.D., and George Quintero, Ph.D., lead the work along with van Horne. It spans the departments of neurosurgery, neuroscience and neurology within the UK College of Medicine.
This work began thanks to philanthropic funding to UK – like many pilot programs, the seed funding allowed researchers the time and resources to develop the study. But last year, the community funded work took a big step forward, with the STAR trial receiving its first ever support from the National Institutes of Health (NIH). The work is a clear example of how when innovative research is paired with philanthropic funds there can be advances of new ideas, ultimately setting them up for larger federal or foundation grants.
“This has really legitimized to some degree of what we have been working to do,” said van Horne.
Now with what they’ve learned up until this point, the LEAP trial seeks to intervene even earlier in Parkinson’s progression, before patients reach the stage where DBS would traditionally be considered. The goal is to determine whether introducing cell-based neurosurgical implants earlier in the disease’s course could slow or even alter its trajectory. The team at UK is the first to look at this approach and just as the STAR trial started out, the LEAP trial is being funded through philanthropic support of pilot programs as well as backing from UK’s Center for Clinical and Translational Science (UK CCTS).
“What we’ve learned is that when people get DBS, their disease is usually farther along,” explained Quintero. “So, the question became—what if we intervene earlier, when there are more viable brain cells left to work with?”
The LEAP trial is groundbreaking in several ways:
- Earlier intervention: Unlike traditional DBS, which is typically reserved for later-stage Parkinson’s patients, LEAP is focused on individuals in earlier stages of the disease.
- Double-blind study: Unlike past open-label studies where patients and researchers knew who received treatment, LEAP will follow a more rigorous double-blind format to eliminate potential placebo effects.
- Multi-center expansion: If successful, the trial could expand beyond UK, reaching other research institutions across the U.S.
“The patients who have participated in DBS-Plus, like Coach Kennedy, have been instrumental in getting us to this point,” Quintero said. “Their willingness to take part in research has helped shape the next phase of Parkinson’s treatment.”
A legacy beyond basketball
For Kennedy, the fight against Parkinson’s is much like the game of basketball itself. It requires adaptability, perseverance and trust in his team — both on and off the court.
“If somebody reads my story and has been recently diagnosed with Parkinson’s, I want them to know this: Don’t let Parkinson’s define you,” Kennedy said. “You can live a good life. You can manage it. Step out in faith.”
As basketball fans across the country tune in for the madness of March, Kennedy’s story offers a different kind of inspiration. He may not be on the sidelines coaching anymore, but his impact — both in the sport and in the medical community — is undeniable.
Just as he once led his teams through tough matchups, he’s now leading the way in the fight against Parkinson’s. And thanks to the work of researchers at UK, that fight is advancing further than ever before.
Research reported in this publication was supported by the National Center for Advancing Translational Science of the National Institutes of Health under Award Number UL1TR001998, and the National Institute on Aging of the National Institutes of Health under Award Number R01AG081356. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
As the state’s flagship, land-grant institution, the University of Kentucky exists to advance the Commonwealth. We do that by preparing the next generation of leaders — placing students at the heart of everything we do — and transforming the lives of Kentuckians through education, research and creative work, service and health care. We pride ourselves on being a catalyst for breakthroughs and a force for healing, a place where ingenuity unfolds. It's all made possible by our people — visionaries, disruptors and pioneers — who make up 200 academic programs, a $476.5 million research and development enterprise and a world-class medical center, all on one campus.